Living with an anal fistula can be exhausting, especially when pain interferes with daily life. fistula pain management focuses on reducing discomfort, preventing infection, and improving quality of life while planning proper treatment. Pain may vary from mild irritation to persistent discomfort that makes sitting, walking, or bowel movements difficult. Understanding how to manage pain correctly helps patients stay comfortable and avoid complications until definitive treatment is done.
“ Pain doesn’t have to control your life. Get clarity, get comfort, get expert help.”
Understanding Anal Fistula Pain and Discomfort
Anal fistula pain usually occurs due to ongoing infection, inflammation, or pressure inside the anal area. The discomfort can be constant or come and go, often worsening during bowel movements or prolonged sitting. Effective fistula pain management is not just about temporary relief—it also helps protect surrounding tissues and prevents the condition from worsening.
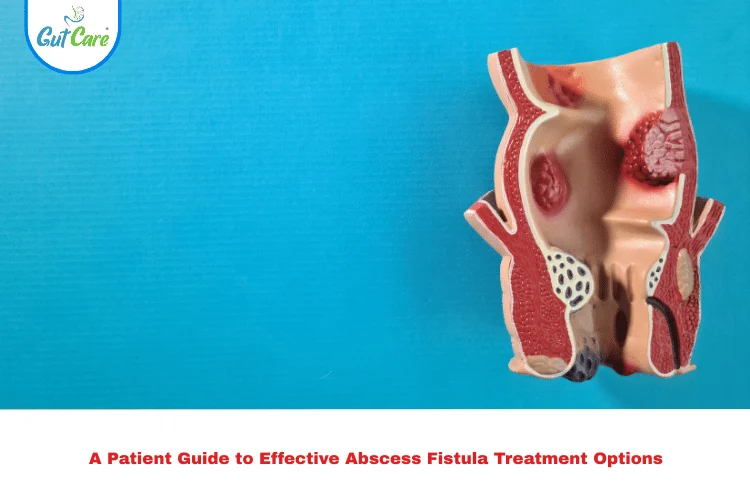
What Is Anal Fistula and Why Does It Cause Pain?
An anal fistula is an abnormal tunnel between the anal canal and the skin near the anus. It usually develops after an abscess does not heal completely. Pain occurs because bacteria continue to irritate the tissues, leading to swelling, pressure, and sensitivity. Without proper fistula pain management, the inflammation can persist and cause repeated flare-ups.
Common Symptoms Associated With Fistula Pain
People with anal fistula pain may notice:
- Persistent soreness near the anus
- Pain while sitting or walking
- Discomfort during bowel movements
- Swelling or irritation around the opening
- Occasional fluid discharge
Recognizing these symptoms early helps guide timely fistula pain management and medical care.
Causes of Severe and Persistent Fistula Pain
Pain becomes severe when infection spreads, drainage gets blocked, or inflammation increases. Delaying treatment or relying only on home care can make pain harder to control. Chronic cases often require structured fistula pain management under medical supervision.
Effective Ways to Reduce Anal Fistula Pain
- Warm sitz baths: Sitting in warm water for 10–15 minutes, 2–3 times a day, helps relax muscles, improve blood flow, and reduce pain and swelling.
- Maintain gentle hygiene: Clean the area with lukewarm water and mild, fragrance-free soap; avoid harsh wiping or scented products.
- Use prescribed pain relievers: Doctor-recommended pain medications or topical ointments can help manage inflammation and discomfort.
- Increase fiber intake: Eating high-fiber foods softens stools, reducing strain and pain during bowel movements.
- Stay well hydrated: Drinking enough water helps prevent constipation and eases bowel movements.
- Avoid prolonged sitting: Use a soft cushion or donut pillow to reduce pressure on the anal area.
- Wear loose, breathable clothing: Cotton underwear helps prevent moisture buildup and skin irritation.
- Follow medical advice promptly: Treating infections early and following treatment plans prevents pain from worsening.
Why Proper Pain Management Is Important in Anal Fistula
Effective pain management improves quality of life for individuals dealing with an anal fistula. Continuous pain can lead to stress, anxiety, and difficulty maintaining hygiene or normal bowel habits. When pain is controlled, patients are more likely to stay active, maintain proper nutrition, and follow medical advice consistently.
Managing pain also helps reduce muscle spasms around the anal sphincter, which can otherwise delay healing. Combined with appropriate medical or surgical care, pain relief measures play a key role in faster recovery and lower risk of recurrence.
Medical Treatments for Fistula Pain Management
Doctors focus on reducing infection and inflammation first. Fistula pain management may include cleaning the tract, controlling infection, and preparing the area for further treatment if needed. Consulting an experienced colorectal surgeon ensures pain is managed safely without masking underlying issues.
Role of Antibiotics in Managing Fistula-Related Pain
Antibiotics are used when infection is active. They help reduce bacterial load and ease pain caused by inflammation. However, antibiotics alone cannot close a fistula, so fistula pain management must be combined with ongoing medical evaluation.
Home Remedies to Relieve Anal Fistula Discomfort
Simple home care plays a strong supportive role in fistula pain management:
- Warm sitz baths to soothe the area
- Gentle cleaning after bowel movements
- Wearing loose, breathable clothing
These steps reduce irritation and improve comfort.
Diet and Bowel Management to Reduce Fistula Pain
A fiber-rich diet helps soften stools and reduces strain. Drinking enough water prevents constipation, which is essential for consistent fistula pain management and daily comfort.
Lifestyle Changes That Help Control Anal Fistula Pain
Avoid prolonged sitting, take short walks, and manage stress. These small adjustments support long-term fistula pain management and reduce pressure on sensitive tissues.
Managing Fistula Pain While Sitting or Walking
Using a soft cushion and changing positions frequently can reduce pressure. Gentle movement improves circulation and supports ongoing fistula pain management.
Fistula Pain During Bowel Movements: How to Reduce It
Pain during bowel movements often signals irritation. Stool softeners and proper diet help minimize discomfort and are key parts of fistula pain management.
When Pain Indicates the Need for Surgical Treatment
Persistent or worsening pain often signals the need for advanced care. Surgical evaluation helps resolve the source of pain rather than only managing symptoms.
Preventing Pain Recurrence After Treatment
Following post-treatment advice, maintaining hygiene, and attending follow-ups help prevent pain from returning. Long-term fistula pain management depends on consistency and care.
When Medical Support Is Needed to Control Anal Fistula Discomfort
While home care can help, persistent or worsening pain should not be ignored. Effective fistula pain management often requires medical evaluation when pain affects sitting, walking, or bowel movements. Ongoing discomfort may indicate active infection or inflammation that needs professional treatment. A colorectal specialist can assess the cause of pain and suggest appropriate solutions, ensuring relief while preventing complications. Seeking timely medical guidance helps manage pain safely and supports long-term recovery.
When to See a Doctor for Fistula Pain
If pain lasts more than a few days, worsens, or affects daily life, medical advice is essential. At Gutcare Clinics in Bangalore, patients receive personalized care guided by Dr. Yuvrajsingh Gehlot, colorectal surgeon, who focuses on comfort, safety, and long-term results.
Risks of Ignoring Persistent Anal Fistula Pain
Ignoring pain can lead to complications, prolonged recovery, and repeated infections. Timely evaluation at Gutcare Clinics helps patients avoid unnecessary suffering and ensures proper treatment planning.
Why Expert Care Matters
Specialized centers like Gutcare Clinics combine experience, patient-first care, and evidence-based treatment. Under the guidance of Dr. Yuvrajsingh Gehlot, patients receive clear explanations, effective pain control, and honest treatment options.
Final Thoughts
Managing anal fistula discomfort requires the right balance of medical care, lifestyle support, and expert guidance. With proper fistula pain management, patients can stay comfortable while moving toward long-term healing.
Frequently Asked Questions
1. How long does anal fistula pain usually last?
Pain duration varies, but proper fistula pain management helps control symptoms until treatment is completed.
2. Can home remedies fully control fistula pain?
Home care supports comfort, but medical evaluation is essential for complete relief.
3. Is surgery always needed for fistula pain?
Not always, but persistent pain often requires surgical assessment.
4. Does diet really help reduce fistula pain?
Yes, diet plays a key role in reducing strain and discomfort.
5. How to relieve fistula pain?
Fistula pain can be relieved with warm sitz baths, proper anal hygiene, a high-fiber diet, adequate hydration, and doctor-prescribed medications to reduce pain and inflammation.